In 2002 the then Labour-Alliance government implemented what was known as the Primary Health Care Strategy.
A key feature was replacing the system of funding general practices from demand driven uncapped government fees (subsidies) to capitation.
Capitation had previously been tried and tested in some parts of Aotearoa New Zealand’s health system, particularly the western Bay of Plenty, but it now became universal. It remains in force today.
What is capitation
In summary capitation in 2002 was based on the numbers of enrolled patients with individual general practices who belonged to the populations of newly established primary health organisations (PHOs).
PHOs and their general practices are paid according to the number of people enrolled instead of, as previously, the number of times a general practice sees a patient.
It is called capitation because it is a per capita payment (ie, per enrolled patient). General practices can supplement their incomes by regulated patient co-payments.
Calculating capitation funding is based on a formula which, in addition to patient numbers, also takes into account two demographic features of the make-up of each general practice’s enrolled population.
The first is age. It recognises that, in general, people need more care both when they are very young and when they get older.
The second is gender. This recognises that women in their child-bearing years tend to need services more frequently than men.
Capitation funding does not differentiate between a doctor or nurse visit. Partly this reduces some unnecessary transaction cost.
But, more important, it recognises that in some cases it recognises that health service provision might be more appropriate by a nurse than a doctor (or a combination).

Capitation principle a lasting legacy of former health minister Annette King
Moving to capitation funding was a substantial improvement for general practices and their enrolled patients. With sound underlying principles, it has been a lasting positive legacy of then health minister Annette King.
Decapitation of capitation beckons
But it is now obvious to almost all in the health system, certainly to general practitioners and their representative bodies, that capitation is in the process of being decapitated.
Capitation heading to decapitation
This is not because of its design. Capitation is much superior to what it replaced. Its underlying per capita principle remains critical.
But, for many years, its ‘engine’ has been neglected by the political and bureaucratic leaderships of the health system. The ‘engine mechanics’ have failed the system.
The health status and demand of New Zealanders has increased dramatically, for the worse, in the over 20 years since capitation funding was implemented. The population has grown. Further, the population is aging meaning more older patients with more comorbidities.
Then we have the worsening external social determinants of health which largely focus on increased poverty and the other consequential drivers of health demand such as low incomes and poor housing.
Taken together, this means that compared with 2002 there now are more patients who are seriously sicker, including those with ongoing debilitating chronic illnesses.
There are now more patients, both in absolute numbers and proportionately, presenting to general practitioners with highly complex conditions. And the trend is going in the wrong direction.
Age and gender remain important but they simply don’t cut it as a means of contributing towards the assessment of what the level of capitation funding should be and how it should be dispersed.
Groundbreaking study of the ‘tyranny of follow-up
One consequence of this is that significantly increased GP workloads have manifested as what has been described as the ‘tyranny of follow-up’.
The light has been shown on this by a groundbreaking study undertaken by the Royal New Zealand College of General Practitioners. It results were released on 4 March: GPs working for free to complete crucial patient follow-up.
The study revealed that for every hour a GP spends face-to-face with a patient, another 30 minutes of clinical follow-up is generated.
Over 56% of GPs’ time is spent on direct patient consultation while nearly 31% to patient related ‘non-clinical’ tasks such as referrals for further investigations and managing laboratory test results.
The biggest component of the remaining 14% is training and education (over 6%). The rest is divided roughly equally between clinical governance and practice management.
Capitation relates to a notional 40-hour week or 10 patient sessions a week. However, once a GP is working six to seven sessions a week (three to three-and-a-half days), in the real world, they have already worked 40 hours. Ten patient sessions would mean 60 rather than 40 hours a week.
What was fairer in 2002 is very unfair in 2024. No longer should the capitation funding formula be left to be to be ultimately determined by the government through Te Whatu Ora (Health New Zealand; previously it was the Ministry of Health).
It needs to be co-designed and agreed between those who act for government (Te Whatu Ora) and those who best know how fairly and effectively the system is working (general practitioner organisations).
Adapted principles for determining capitation funding formula
It would do no harm to look across to the system of remuneration for salaried senior doctors and dentists previously employed by district health boards and now by Te Whatu Ora.
One of the things that I successfully advocated for, when executive director of the Association of Salaried Medical Specialists, was the inclusion in the national collective agreement of strong intertwined clauses on hours of work, job sizing, and time for non-clinical duties. They are still in force today.

Importance of protecting working hours
Hours of work were required to be mutually agreed. Job sizing was the average time to undertake duties and responsibilities. These included routine duties (normally in a Monday-Friday week), hours worked on an after-hours call roster, and time for non-clinical duties.
Non-clinical duties were defined differently from the above-discussed College study. They were for duties not directly related to the treatment of individual patients, such as professional development.
The collective agreement incorporated a recommendation of the Council of Medical Colleges that these duties comprise a minimum of 30% of the job size (excluding after-hours rosters).
These clauses were not always honoured by the employing authorities but they were firm explicit entitlements nevertheless.
The Council of Trade Unions has noted that they are the strongest working hours protections in a collective agreement that it is aware of.
Obviously the details and the process for achievement of these entitlements can’t be mechanistically transferred into a capitation funding arrangement. It applies to employees through a formal collective bargaining process.
Instead capitation applies to subsidies for both for-profit and not-for-profit organisations (general practices) responsible for providing healthcare as part of a universal public system.
However, the underlying principles could be applied by developing a fit-for-purpose capitation funding formula based on co-design and mutual agreement between government (Te Whatu Ora) and the relevant GP organisations.
Patients and their health system and patients deserve a capitation system that addresses the higher patient complexities and volumes of 2024, not the lesser ones of 2002.
Ian Powell was Executive Director of the Association of Salaried Medical Specialists, the professional union representing senior doctors and dentists in New Zealand, for over 30 years, until December 2019. He is now a health systems, labour market, and political commentator living in the small river estuary community of Otaihanga (the place by the tide). First published at Otaihanga Second Opinion





A really good report. I found that the health system as I have experienced has helped me through problems. One child with chronic fatigue syndrome was a problem because it was hard to establish the cause at first, and then get a way forward. We did! I got the help I needed both from the GPs and through being able to get a wee bit of assistance to see specialists quickly. Who helped as much as possible.
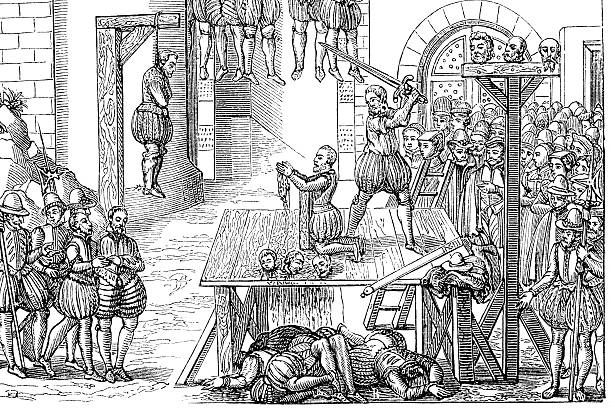
NZ/AO is going backwards and I like your cartoon of an ancient slaughter house. They did things physically and we hurt people psychologically instead I think. Helping individuals to make goals that are achievable and then be rewarded with satisfaction and some other pleasure, would reduce the pervasive illness at all ages. But we have a moribund political system now having have replaced one with a semblance of spirit, with one depressingly unsatisfactory. So thanks Ian Powell for explaining how things are as there is a fog of bland misunderstanding even ignorance about our impossible expectations confronting mendacios policies.
The PHO model wasn’t necessarily all that good per se. Much specialist care or attention was devolved back onto general practitioners/family doctors, who themselves said that they didn’t have the training or expertise to be making some decisions eg like if a “client” needed a colonoscopy.
Specialists are precisely that, but the philosophy of the PHO appeared geared to cut back routine public hospital services, although they’re still pretty good in emergencies. The fact that public hospitals now have customer service reps to process GP referrals, rather than trained medical people,
can’t be described as best practice. And if a GP is a lousy letter writer, it’s even worse.
Interesting Snow White – you sound as if you know about the situation.
My relation was involved working in a clinic in Auckland and noticed how many people want to pile into the medical system once they have arrived to live here from overseas. I’m concerned that is one of the advantages attracting people here and causing them to pay what are high fees for the pleasure. We may not front up afterwards with the promised services. And NZs are pushed back – like we aren’t really top priority in the country we live in.