General Practice New Zealand (GPNZ) is an interesting organisation formed over a decade ago. General practitioner representation is fragmented in Aotearoa New Zealand but GPNZ’s formation did not add to the fragmentation. Instead it provides a voice for networks of general practices rather than individual GPs.
In April 2019, GPNZ published a thoughtful discussion paper. Titled Workforce and resources for future general practice, the paper deliberately does not address specific future business models and governance. In some respects this is disappointing but it does ensure that its main focus is not diluted by these matters
Workforce model and responsiveness
What GPNZ does is describe a model in workforce terms. It lists requirements for responsiveness in order to ensure an improved and comprehensive primary care service for New Zealanders.
These responsiveness requirements are defined as:
- unmet need
- recognition of the changing roles and career expectations of medical practitioners
- building upon emerging workforce roles
- building primary healthcare teams that have a wider range of capability than is currently the norm, and
- articulating an approach that can be implemented widely across different communities, with a high degree of local responsiveness and local variation where appropriate.
Extended primary care team
GPNZ promotes greater integration within a structure it labels “extended primary care teams”. The high-needs Porirua Union & Community Health Centre is used as a current example.
Its model outlines the staff needed for 10,000 enrolled patients. For a general-needs population, this would require 31.3 full-time equivalents; for a high-needs population, 42.5 would be required. The difference would largely be in additional nurse practitioners, GPs, social workers and reception/administration.
The usefulness of this is model is that it indicates the additional workforce investment needed to cater for a high-needs population would be around 35%.
In thinking about the paper generates consideration of other issues. One is integration. Another is governance.
Integration
The current dominant general practice model is limited in its ability to provide accessible and equitable access to quality primary healthcare, as the foundation of a health system intended to produce a universal public good.
GP-owned practices have done Aotearoa New Zealand well, with strengths that should be retained, whichever way primary care evolves. But its small-business structure means there are limitations in its scope to reach out to everybody, particularly those in economically deprived or smaller, isolated communities (ie, high health needs).
Further, largely generationally driven, GP practice partners are declining and upcoming doctors have less interest in purchasing the equity of a retiring partner. There is a limit to the extent existing partners can buy up this equity. Realistically, only corporates can fill this gap if private ownership is to remain the norm.
While improving integration within primary care is essential (as advocated by GPNZ), why stop there? Why not improve integration between primary and secondary care (ie, between today’s GP surgery and hospital) to a level that makes good clinical and wellbeing sense?
Governance
Improving integration within general practices and between it and hospitals leads on to the issue of governance – which GPNZ avoids (understandably, if its paper is seen as part of developmental thinking). Governance should not be left as the elephant in the room.
Consequently, the term “polyclinics” entered my cognitive processes. I had a positive glimpse of them in the Netherlands many years ago.
Over a decade ago, I observed a top-down, one-size-fits-all attempt to introduce them in the National Health Service in England, which included potential private corporate takeover. There was a glimmer of a good idea behind them, but the execution was a shocker. Failure was the outcome.
Cuba
What really prompted my thinking was visiting Cuba in January 2020. There are three main structural tiers to the Cuban health system: community based polyclinics, general secondary care hospitals and sub-specialist tertiary hospitals.
There are nearly 500 polyclinics across the island, each serving defined populations of between 20,000 and 60,000 people. They have a strong neighbourhood flavour about them.
Population size-wise, Cuban polyclinics are comparable with New Zealand’s smaller district health boards (DHBs) such as Tairāwhiti, Wairarapa and West Coast (a little smaller than Whanganui and South Canterbury). It means that they probably know their populations better than most DHBs know theirs. Being well staffed (with doctors and nurses, especially), Cuban polyclinics have the capacity to mobilise to ensure visits to each home annually for immunisation.
Owing to the highly punitive economic blockade from the US, it was necessary for Cuba to develop its own Covid-19 vaccines. Its polyclinics provide better vaccine distribution to their populations than is seen in many other countries.
Polyclinics don’t just provide primary care. They extend into areas of sub-acute hospital care (less so surgery), including outpatient clinics and treatments with the necessary diagnostic support required.
Embryos?
There is no equivalent to these polyclinics in New Zealand. The closest example I can think of is Southern DHB’s Lakes District Hospital, in Queenstown, with the extensive use of rural hospital medicine specialists and visiting specialists from Dunedin and Invercargill. However, primary care is provided by two local general practices. The nearby community trust-run Dunstan Hospital in Clyde is in a similar situation.
It is possible that Taranaki DHB’s initiative to establish a new medical centre in Hawera, staffed by rural hospital medicine specialists and providing a range of primary and secondary care, might have been an embryonic polyclinic.
But the DHB’s engagement with local general practices was a flop. If polyclinics were to be considered in New Zealand, engagement must be of a much higher standard.
Polyclinics in Aotearoa?
Should polyclinics be seriously considered for New Zealand? I think so, provided their structure follows design and the design recognises both the prevalence and provision of quality care of general practices in Aotearoa.
So design should not be one-size-fits-all. Its focus should be on access, not just to primary care but also to hospital outpatient clinics and some other sub-acute work that could sensibly be undertaken in a more local setting. Inclusion of pharmacy and dentistry should not be ruled out, depending on the state of local access.
The growing relatively new branch of specialist medicine known as rural hospital medicine with its emphasis on episodic care offers opportunities that should be considered. Rural hospital medicine specialists can be increasingly found in small DHB or community trust owned hospitals from Northland DHB down to Southern DHB.
But design must also recognise that polyclinics should not compete with privately owned general practices. Cooperation and collaboration have to be the governing ethos.
Governance must be addressed as part of design. DHBs would be the logical statutory bodies to assume overall ownership if the Government were not still foolishly determined to dismantle them in the midst of a raging pandemic!
If DHBs are replaced by the proposed new national health bureaucracy currently called ‘Health New Zealand’, then it should assume ownership (despite its highly bureaucratic centralised nature).
The only other option for polyclinics of this kind would be private corporates. But they are less inclined to invest in less profitable or unprofitable deprived or isolated populations. Given that the Government has little idea what will replace DHBs in community care responsibility there is serious risk of a governance vacuum being created that will allow corporates to suck up and takeover these fragmented bits.
Although the quality of political leadership of the health system does not inspire confidence, this is no justification for not advocating correcting primary care’s pending governance deficit.
[This blog is a revised version of my regular column published by New Zealand Doctor on 10 November 2021]
Ian Powell was Executive Director of the Association of Salaried Medical Specialists, the professional union representing senior doctors and dentists in New Zealand, for over 30 years, until December 2019. He is now a health systems, labour market, and political commentator living in the small river estuary community of Otaihanga (the place by the tide). First published at Otaihanga Second Opinion




What ever comes after the DHB will be the same debacle as the DHB. Underfunded – by Labour and National alike, understaffed and underapid – under Labour and National alike, under resourced by Labour and National alike.
How comfortable are you currently with the Healthcare sector and your expectation of receiving health care rather then just a script to mask pain?
How comfortable are you thinking that should you get ill vey badly, Covid or othe – will there be an ICU bed for you and more importantly does that bed come with a specialist Nursed trained in ICU care?
If like me you don’t count on getting one of these magical beds but will rather be forced to sit your Covid out at home, blame Labour.
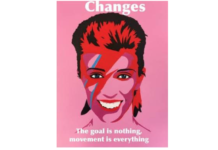
They are now in the second year of their second term, a full majority, and that little man on the image shown above, did his darnest best to not invest, not lift pay for nurses, not hire nurses, not hire doctors and thus the whole country is in deep shit on the eve of a major break out of Delta.
The “failing” DHB were a gift from Helen Clark and the same dull knight’s that are now running the show under Jacinda Ardern.
Anyone who thinks that these guys will be fixing anything needs his / her / its / their/ eyesight’s fixed.
Put those Polyclinics in schools to cover the whole family, plus with the dental clinics at some schools, get a lot more coverage for the community.
I think coupling up the GP’s more with the hospitals is a good idea.
But NZ needs to fully integrate their bizarre policies across the spectrum. In particular their interest in fast food, liquor stores and smuggled contraband like drugs and cigarettes, which seems to be expanding in NZ, led by the ability to buy these businesses and get NZ residency off them. NZ already has a big problem with obesity and diabetes, cancer, mental health and drugs, now getting worse.
The lack of tie in with ‘businesses’ being encouraged into NZ for decades with residency handouts, who have negative social responsibility in mind and victimises people into poor habits, is glaringly obvious.
The Greens in particular (and maybe this article has something to do with it https://thedailyblog.co.nz/2021/11/14/if-radio-nz-banned-hooton-for-conflicts-of-interest-why-not-woke-wellington-general-neale-jones/) have gone off the deep end and seem desperate to get as many high needs people into NZ to compete with other increasingly high needs existing NZer’s.
This of course will lead to big pay offs for the new ‘social bond’ type businesses in housing, rehabilitation, mental health, gender realignment, prisons, cultural work, more translators and others benefiting off more NZ policy led, social disfunction in NZ.
‘
It will also lead to record debts for NZ to try and navigate this expanded group of people of very high needs across the spectrum and needing more and more non core workers operating in that space (aka more translators in hospitals, justice, more lawsuits and complaints etc)
Much of this is covered up and the front line health workers blamed, who in NZ are leaving (GP’s, doctors, nurses).
In spite of low Covid rates in NZ, ‘nurse Jenny’ came here for a holiday, not to work as our pay rates, and dysfunction in our hospital system, inability to retain experts and professionals, has got too much for many experts.
50% of our doctors are GP’s, many are retiring and who is going to replace them?
Theirs seems to be a racial agenda on this as British doctors (used to world leading free health systems) are out of favour. The woke prefer criminals and those from paid/private health systems in the DHB’s.
Emails reveal residency pleas of rural GP, convicted criminals granted stay
https://www.newstalkzb.co.nz/news/politics/residency-limbo-emails-reveal-pleas-of-rural-gp-while-convicted-criminals-granted-stay/
Doctor excluded from one-off residence visa says govt change ‘makes no sense’
https://www.rnz.co.nz/news/national/454310/doctor-excluded-from-one-off-residence-visa-says-govt-change-makes-no-sense
Government immigration policy seem to be removing British doctors who are already in NZ and qualified and working, to bring in doctors from overseas who may not even meet the requirements in NZ while wanting more criminals and high needs people here.
It is interesting for someone who has just had a largeish procedure that has drawn on integration between DHBs ie between a ‘primary’ advanced procedure hospital and an adjoining feeder hospital which carries out initial tests and aftercare. I have access people helping me shower and wound dressing district nurse to whom I questioned about her knowledge of why I get occasionally dizzy. She is arranging a visit from someone to test my blood flow which is probably restricted to my leg. So she can act and I can ask, and I keep in touch with the GP and may talk to the nurse, and have had phone consultations with the doctor. I have a 3 month phone consultation with the heart department at DHB in place soon.
This system operating at present seems excellent in supporting the patient at home. Incontinence and a bout of bronchitis have been dealt with effectively on top of the main considerations. Gaining district and home care can relieve pressure on the workforce and its buildings.
GPs might be encouraged to go to rural areas as the old bonded system. Also they need to have the chance to find a partner in life from amongst the people they care for; the present puritan requirements are too demanding, there needs to be a board which the GP can argue a case to.
I have read a series of fiction books based on the life of a USA ‘district nurse’ which seems different to what we do, but seems to be most useful to them. The Sue Barton series was written for adolescent girls, fiction but with fact at the back, written that way. https://en.wikipedia.org/wiki/Sue_Barton
It introduces too the – https://en.wikipedia.org/wiki/Henry_Street_Settlement
These sort of books would help in drawing attention of practical girls who want a career.
It seems to me that the role of GPs needs to be glamorised, being one is as exciting and demanding as climbing Mt Everest and Hillary is still remembered for that. Dramatise the position and its importance and wide knowledge and numbers will creep up with other changes and improvements made. I have books about medical people, one particularly about Dr Smith from Rawene in the early 1900s, fascinating and interesting and a matter of pride to Alexander McCall Smith, the medical ethicist and author. It isn’t a boring life, so improvements to the methods should bring more practitioners, especially partnerships and group practices.
Yes Greywarbler I agree, a bit of glamorising could help attract new recruits and also lift community awareness of the role. I still remember the excellent TV series ‘Country GP’, almost as good as Country Calendar!
It seems to me that an only partially government funded GP system, based around private practices, will not provide for financially deprived areas. Without incentives and support medical staff will not be attracted to invest in those areas. First we need to train more doctors and nurses; bonded scholarships could help many to train.
I like the concept of local hospitals establishing your idea of ‘polyclinics’ where bonded students could be placed and employed on salary. The autonomy, variety, and absence of need to invest financially may also attract many to these roles.
savenz 8.55am Looking at and in a complete circle around our problems, brings up some difficulties that will, not may, arrive in the future if not already showing.
This of course will lead to big pay offs for the new ‘social bond’ type businesses in housing, rehabilitation, mental health, gender realignment, prisons, cultural work, more translators and others benefiting off more NZ policy led, social disfunction in NZ.
It will also lead to record debts for NZ to try and navigate this expanded group of people of very high needs across the spectrum and needing more and more non core workers operating in that space (aka more translators in hospitals, justice, more lawsuits and complaints etc)
A bit of a beat up of government, but after the emotive case recently of the man dying of Covid in West Auckland in the Herald, that failed to disclose he had not been vaccinated or any of the other family members, am now having distrust of the reporting of this issue. If people refuse vaccination and treatment, then the family should not be putting the blame on health services.
Saying that, whtywould they expect patients with Covid to call Healthline?. It’s not a good service a lot of the time, and apparently very hard to get hold of and no doctors. It makes more sense to arrange for the local GP to call, as they are a doctor!!!!
You have to wonder why they can’t work this out for SIQ. https://www.nzherald.co.nz/nz/covid-19-delta-outbreak-miq-transiting-to-siq-a-sensible-and-necessary-response-but-needs-to-be-fit-for-purpose/O6CQT57RPNH5FLXATI6JYBSJYI/
During lockdown we used our GP and they were fantastic on the phone service.
indeed we must start blaming the numpties for their own fate ‘free to be dumb’ means consequences, there are no barriers to getting vaxxed so if you don’t – on your head be it…and that needs to be highlighted in flouro and double underlined in red sharpie.
the detail of organisation within any public service is immaterial if that service continues to be chronically underfunded…the debate is fruitless unless someone stumps up
Totally agree gagarin. The MSM need to step up and bluntly ask these questions; if someone is making a public issue of a perceived failure in the public system the public have a right to know all the facts. Once someone goes public with an issue it must be made possible for the accused government department to respond publicly.
Yes also agree no amount of restructuring will solve problems if the underlying cause is under-funding; but I wonder how much government spending is lost in the administration and never sees it to the ‘coal face’.
Comments are closed.