Research over many years has identified serious longstanding health inequities for tamariki (Māori children). This has been both reinforced and updated by new recently published research by the Universities of Auckland and Otago.
These latest findings were reported in Te Ao Māori News on 25 January: Māori children suffering most from health inequities.
Research findings
The research found that Māori children are unable to engage with primary healthcare, outpatient care, medicines and laboratory investigation to the same degree as non-Māori. Consequently the finding that tamariki have higher rates of avoidable hospitalisations and deaths than other children is no surprise.
The Royal New Zealand College of General Practitioners has rightly called for urgent action to reduce these health inequities. Also rightly, it notes that the findings are neither new nor surprising. With precision the College concludes that this lack of newness and surprise in the findings is exactly the problem. The College has got it in one.
Health inequities go beyond primary care and access to general practice. It is also hospitals. This is confirmed by the invaluable New Zealand Health Survey which the Ministry of Health publishes annually.

Invaluable and revealing annual New Zealand health survey
The 2019-20 survey revealed that Māori adults had the highest prevalence of not being able to book an appointment at their usual general practice within 24 hours.
When access to general practice is delayed or blocked due to factors such as cost and social determinants of health, this has harmful flow-on effects for the whole whānau. General practitioner diagnosis is also crucial for Māori to access hospital care.
Getting function and form right
Two things become clear from various research findings, including the most recent discussed above, over Māori health inequities. First, there is no one-size-fits-all solution to address them. If there was then it would have been found by now.
Second, despite best endeavours, at a national level the structure responsible for addressing them was not fit-for-purpose. In terms of the critical relationship between function and form in health systems, the function was identified (health inequities) which then led on to consideration of the form (structure).
This is where Te Ake Whai Ora (Māori Health Authority) comes in. The Heather Simpson led review of the health and disability system recommended in 2020 the establishment of such an authority but limited to an advisory role.
However, the review’s final report also included a section by dissenting review members recommending a much stronger role for the authority. Ironically they were the majority but, as Simpson was reported as saying, the majority position does not mean that it is the review’s position (at least, I opine, not a review chaired by her).

Andrew Little deserves credit for establishing Te Ake Whai Ora
To his credit (and it is the only thing I will give him credit for as health minister) Andrew Little supported the review’s ‘majority’ position. He then proceeded to progress it through Parliament as an important part of the Pae Ora Act, which took effect on 1 July 2022.
Māori Health Authority: objectives and functions
Under the Act the objectives of the Authority are to:
- ensure that planning and service delivery respond to the aspirations and needs of whānau, hapū, iwi, and Māori in general;
- design, deliver, and arrange services; and
- promote Māori health and prevent, reduce, and delay the onset of ill-health for Māori.
These three objectives are followed by several functions which include:
- jointly developing and implementing a New Zealand Health Plan with Health New Zealand;
- owning and operating services;
- improving service delivery and outcomes for Māori at all levels of the health sector;
- collaborating with other agencies, organisations, and individuals to improve health and wellbeing outcomes for Māori and to address the wider determinants of health for Māori;
- providing accessible and understandable information to Māori on the performance of the publicly funded health sector;
- commissioning kaupapa Māori services and other services developed for Māori;
- reviewing locality plans developed by Health New Zealand;
- undertaking and promoting public health measures, including commissioning services to deliver public health programmes;
- providing policy and strategy advice to the Minister of Health on matters relevant to hauora Māori;
- designing and delivering programmes for the purpose of improving the capability and capacity of Māori health providers and workforce; and
- undertaking and supporting research.
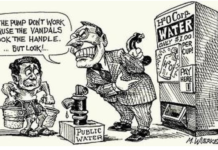
The nonsense of separatism
These objectives and functions give Te Ake Whai Ora considerable power and influence at various levels in the health system in order to address the difficult and complex challenge of Māori health inequalities.
Power and influence is in how Māori healthcare and wellbeing are planned, designed, developed and delivered. This includes its own direct role in ‘hands-on’ delivery. Further, beyond diagnosis and treatment, there is a strong population health emphasis which is essential for medium to long-term Māori health planning.
The opposition to the Māori Health Authority is based on an opportunist argument of separatism; that is, a second separate health system is being established for Māori. This opposition is primarily from the National, Act and NZ First parties, although the far right is also in this chorus singing from the same tuneless song sheet.
Within the spectrum of what might constitute nonsense, this separatism argument is at the extreme end of nonsensical. At best it is a misleading soundbite.
Much of the focus of Te Ake Whai Ora is in communities and with primary care where many Māori organisations are already active. The expression ‘by Māori and for Māori’ is commonly used and has been uncontentious for both National and Labour-led governments.

Riana Manuel, Chief Executive, Te Ake Whai Ora
The purpose of Te Ake Whai Ora is to build on this in order to sharpen and enhance the capacities and capabilities required to address Māori health inequities. This is not separatism in community based healthcare. Nor is it establishing separate hospitals for Māori (critical mass alone makes this a nonsense).
Instead, creating the Authority is about adjusting structures to better align with the diversity of health statuses which include significant and disproportionate disadvantages.
An additional moral in the story
Establishing the Māori Health Authority is a good example of form following function. It is unfortunately that in much of the Government’s other health restructuring, form comes first leaving function to be poorly thought-out
The Simpson review (both its ‘official’ and ‘majority’ positions) envisaged that the Authority’s work would be supported by district health boards. This would have been invaluable because of their focus on and experience with the healthcare needs of their geographically defined populations.
DHBs would have been an excellent resource for the Authority to draw upon. Their abolition has meant that this has been hugely downgraded by a much more vertical structure.
This thoughtlessness will make Te Ake Whai Ora’s effectiveness more difficult to achieve. It already has enough difficulties with things it has no control over such as external social determinants of health. While this is no reason for not trying, it is a pity nevertheless.
Ian Powell was Executive Director of the Association of Salaried Medical Specialists, the professional union representing senior doctors and dentists in New Zealand, for over 30 years, until December 2019. He is now a health systems, labour market, and political commentator living in the small river estuary community of Otaihanga (the place by the tide). First published at Otaihanga Second Opinion




And what of Pacifika Ian? Their stats are equally appalling.
I still maintain that not proceeding from a universal approach is quite wrong, and has the potential to devolve into mindless racial chauvanism.
‘By Māori and for Māori’ may well be a phrase used by both political parties, but it is a racialist idea from a bygone era. In a racially integrated society, it should not matter what the race of the physician or his secretary is — but rather providing service in all local languages is the focus.
The issue of ‘not being able to book an appointment at the usual general practice’ has two aspects. One is the failure of government to maintain the promise of fee-free primary care visits as part of the Social Security system (such visits were once bulk-billed to the state). The other is the abolition of the free primary care clinics, once operated directly by the state, and thereby reducing supply of general practitioners.
In regards to access at hospitals, this is a function of the decision to shut down regional hospitals, and close emergency rooms in certain metropolitan areas.
Regular, compulsory physical examinations by state nurses in the schools, colleges and workplaces would further increase access.
Ultimately the root cause of these inequalities lies in the exploitation of working people. Black workers are more likely to be in the lowest strata of the working class, and often live in terrible conditions — their brothers, the poorest of the white workers, need just as much help.
Agreed Kristoff – Health should be delivered on the basis of need, not race.
@Kristoff agreed I suspect the process goes something like this
Problem: Health outcomes are worst for the working class. A greater proportion of the maori population are working class so maori heath outcomes are worse than for other racial groups.
Solution: Build special facilities for maori.
Result: Middle class and upper class maori are best placed to take advantage of the new facilities.
Prediction: Health outcomes are worst for the working class. A greater proportion of the maori population are working class.
Repeat.
A race based analysis risks lazy and fashionable policy making. How do low income maori compare with low income pakeha. What about urban compared to rural etc? If the problem is genuinely race based then fine but typically income and postcode tend to be far more predictive of outcomes than race and there may be other factors to consider.
The intersectional view seems to stop at ‘proving’ a simplistic oppressed/oppressed model. If it meant multifactor analysis in a meaningful sense I could get behind it.
Equally appalling in terms of what? Representation in disease area stats or actual outcomes? There is a difference
Equally appalling in terms of what? Representation in disease area stats or actual outcomes? There is a difference
The MHA clearly isn’t separatism because it is being paid for out of the same consolidated revenue the main health system is paid for.
Also, will the MHA’s managers and leaders be held any more accountable for their system’s performance than the ones currently in charge of our system now? Fat chance….
If it’s not going to provide separate facilities and it will employ the same people as in the general health system, how is it going to achieve anything other than add overhead through bureaucracy?
Of course if other demographics were as unhealthy on average as Maaori, we would have solved the “inequity” problem, wouldn’t we?
People can’t even access healthcare, how would they know how unhealthy anyone is? Did they even look at anyone other than Maori to actually make the comparison, or is it just assumption?
Yes PP – as Churchill noted the marvelous thing about socialism is it assures an equal sharing of misery.
I wasn’t bagging socialism. My point was that the term “health inequity” is at best intellectually negligent, at worst outright knavery.
NO-ONE has these things, why should only Maori have these things?
Especially GP access within 24 hours – I don’t know anyone who has access short of /months/, and that’s if you’re lucky enough to even find a GP with an open roll.
The Maori health authority is insulting and racist because these issues exist for everyone.
100% mods. I was a poor pakeha kid. We ALL need this shit.
My major comment would be – was socioeconomic factors taken into account when conducting research surrounding Maori health? I believe there is a real reluctance to acknowledge that Maori are disparate and that -possibly – the inequity for Maori health are a result of a large proportion of them in poverty not race: correlation not causation (because they don’t want to be considered rascist). If this is the case, and it is not acknowledged, there is likely it be middle class capture of any steps to address this, where as a focus on those poor, rural peoples could really make a difference. As Rev Barber of the Poor Peoples Campaign “When you lift the lowest boat, you lift all boats”
I also don’t have a problem with Te Ake Wha Ora as long as they are willing to look into this and put their money into helping their people who are really needing this extra help not just general – which will result in these people still being disadvantaged
Access to health care is more a class than ethnic issue.
Astonishing the amount of abused children who end up in hospital whose parents go to McDonalds first.
Instead of needing a dual health system for woke thinkers, maybe spend the time to make sure that the current one is better resourced for all.
It is not the health cares fault when parents either hide their kids injuries or go to McD’s first. Mostly it is a class issue.
It is not the health cares fault when Maori are living in un healthy motels and hotels or Kainga ora state houses that have not been upgraded or if the tenants are attacking their neighbours and own housing, bringing their kids up in gang and meth houses or suffer family abuse.
Poor diet is a big issue, obesity, smoking, diabetes. Having liquor shops in every corner, hugs for drug smugglers and highly processed food as the staple in supermarkets isn’t helping.
Most of NZ’s issues are class based – government have spent a fortune on all these dual care for Maori but little to show for it, in fact it seems to be getting worse as a lack of responsibility and sense of entitlement in gang circles which is growing, is empowered by woke and government to accept that kids will grow up like that with those values.
I believe there is institutional racism, but the woke reverse racists is becoming a joke where every problem is now blamed on colonial imperialism and a hand out for more and more money being siphoned off by people who now demand it or using it to self profit or pet projects. The money isn’t getting to the people who need it, that is for sure!
The only way to overcome class is quality education, but the down scaling and anti science woke mantra in NZ education is making kids in NZ less educated and falling behind international circles with unqualified people on subject matter, making up the information leading with race not international knowledge. It is not going to help train more doctors and nurses, they won’t have the education to actually get into our few places with our education system being based on attracting international money now anyway not local skills.
Agree save NZ
At a time when both money and staff are in short supply why are we duplicating health needs .Pakeha, Maori, Pacifica, Asian,Indian all bleed the same blood have the same aches and pain and the same mental needs.
Incorrect. 69% of those suffering mental health issues are represented by Maori. So no, we don’t all bleed the same.
It will be sometime till we see if this initiative has worked or not.
Like so many issues we have likely failed to identify why Maori health stats are so poor.
A genuine question? If you do a class based analysis how do the stats compare?
Not everyone exhibits the same behaviour, and this applies to groups of people as well. Behaviour as an input, leads to certain outputs. It is a simple matter of causality.
The problem here isn’t that Maori (be they children or adults) don’t have access to healthcare if they need it, the problem is (in terms of group averages) Maori lead more unhealthy lifestyles than others. Of course you will see worse health outcomes when the inputs differ. The same applies with something like lower education achievement by Maori: if you don’t do the work, you won’t get good results.
Maori can be given all of the special attention and targeted services in the world, but if they don’t change their behaviour at the level of inputs, then outcomes will never change.
That is a ridiculously simplistic take on a complicated issue.
Look at MS. New Zealand is a high risk country in general but the prevalence in Māori is way lower than those of European descent. Should we cut spend ( granted PHARMAC are tight arses) on all those white folk for being “unhealthy”
Where did Antoine suggest the government “cut spending” to unhealthy people? If you strawman people’s arguments you can’t expect to be taken seriously. I agree her take is overly simplistic. Poor Maaori health is associated with a whole complex of upstream factors including genetics (more prone to obesity, diabetes and gout), socioeconomic and lifestyle factors. Maaori are more likely to be born in poverty, more likely to grow up fatherless, less likely to attend school regularly (that stats are grim), and less well-educated than non-Maaori. These upstream factors MUST influence Maaori health outcomes, and the progressive attribution of poor Maaori health to “systemic racism” in the health system is frankly dishonest.
What Strawman argument? Is it not implied that it’s a waste of resources targeting people who don’t look after themselves? That’s essentially what was said. My point was there are underlying health conditions that are nothing to do with lifestyle. Being put in damp housing as an adolescent and suffering the associated rheumatic complications is not a lifestyle choice.
“It’s not systemic racism when we do it”
if it’s to be funded from the common pot using the same staff and physical resources what is the maori content? another layer of admin and new notepaper?
I am very interested in the research done in the Dunedin Longitudinal study, which showed that people who demonstrated less self control as young as three, showed power outcomes income wise, had higher rates of criminal behaviour, drug abuse and gambling problems. They also had pooper health outcomes. This makes a lot of sense to me and this discovery should be used to improve outcomes